Abstract
COVID-19 has threatened human lives. Countries have implemented various interventions such as vaccination, mask-wearing, body temperature screening, and isolation. However, the effectiveness of single and combined interventions has not yet been accurately analyzed. In this study, an improved SEIR model considering both real human indoor close contact behaviors and susceptibility to COVID-19 was established. Taking Hong Kong as an example, a quantitative assessment of the relationship between the efficiency of single and combined interventions and implementation time and intensity was carried out. The results showed that the infection risk (one-hour close contact with an infected person) of COVID-19 of students, workers, and non-workers/non-students was 3.1%, 8.7%, and 13.6%, respectively. Workplace closures were more effective among built environment interventions. If mask-wearing was mandatorily required in schools, workplaces, supermarkets, shopping centers, and public transport, COVID-19 could not be totally restricted. Workers should be prioritized for vaccination, followed by non-workers/non-students and students. Among all interventions, reducing close contact rate and increasing vaccination rate were better interventions. There was no COVID-19 outbreak (basic reproduction number R0 = 1) if the close contact reduction rate was 59.9% or the vaccination rate reached 89.5%. The results may provide scientific support for COVID-19 prevention and control.
1. Introduction
Since December 2019, the coronavirus disease 2019 (COVID-19) pandemic has been threatening societies, health systems, and economies. As at the end of 2021, over 279 million people have been infected and 5.4 million have died in more than 230 countries worldwide [1]. There have been about 131 thousand infections and 5.7 thousand deaths in China [1]. Until now, global economic losses of at least USD 10 trillion have been caused due to COVID-19, 60% higher than the direct impact of the global financial crisis in 2008 [2].
Airborne (long-range and short-range), droplets, surface, and fecal–oral routes are the potential transmission routes of COVID-19 [3,4,5,6]. Among these, close contact (including short-range airborne and large droplets) is considered to be the main route of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmission [5]. It has been reported that more than 99% of COVID-19 infections occurred in built environment as a result of high population density and long period of time in close contact [7]. In the US, at least 26,000 COVID-19 infections were reported at over 750 colleges and universities on 26 August 2020 [8]. On 24 January 2020, a COVID-19 outbreak in a restaurant caused 10 confirmed cases in Guangzhou, China [9]. In February 2020, an outbreak in a shopping center caused 40 confirmed COVID-19 cases in Tianjin, China [10]. Therefore, built environments face a higher risk of COVID-19 transmission [11] and it has been essential to implement interventions to prevent COVID-19 transmission via close contacts. Until now, countries have implemented a series of interventions, such as quarantines [12,13], built environment closure-related interventions (e.g., school/workplace/entertainment closures, stay-at-home orders) [14,15], body temperature screening in public places [16], isolation of patients [17], wearing masks [14,15], and social distancing [15]. After completing Phase III clinical trials of the COVID-19 vaccines, governments around the world began to encourage people to vaccinate [18,19].
The COVID-19 pandemic influenced the daily commutes of all people during 2020. The pandemic had serious negative impacts on many industries such as construction, tourism, and business [20]. Therefore, in an effort to address the impact of the COVID-19 pandemic, mathematical modeling of transmission under different scenarios was a feasible and timely way to assess the efficiency of interventions on COVID-19 prevention and control. The susceptible–exposed–infectious–removed (SEIR) model has usually been used for analysis of COVID-19 transmission [11,21,22]. Many studies adopted hypothesized human close contact behaviors and ignored the susceptibility of different population groups, and it was difficult to obtain accurate results on the efficiency of interventions [11,21,22]. In addition, most studies [11,22] only considered the efficiency of single intervention, such as school closures, workplace closures, mask-wearing, and social distancing, while ignoring the combination of interventions. Therefore, accurate and comprehensive analysis of the efficiency of interventions based on real human close contact behaviors is urgently needed and important for preventing COVID-19 transmission.
Given the deficiencies of the research mentioned above, this study adopted an improved SEIR model considering both real close contact behaviors of three population groups (student, worker, non-worker/non-student) in seven typical built environments (school, workplace, home, supermarket, public transport, shopping center, restaurant) and susceptibility of different people. Taking Hong Kong as an example, the COVID-19 transmission was simulated. The efficiency of single and combined interventions, such as built environment closure-related interventions, mask-wearing, vaccination, close contact reduction, nucleic acid testing (NAT), and body temperature screening in public places, in terms of implementation time and intensity, was evaluated.
2. Methods
2.1. Model Establishment
The SEIR model has been widely used in infectious disease transmission [11,21,22]. Based on a previous study [22], an improved SEIR model considering both real close contact behaviors (number of contacted people, duration, contact pattern among different population groups) and susceptibility of three population groups (student, worker, non-worker/non-student) was established. Taking Hong Kong as an example, the COVID-19 transmission with different interventions was simulated and the efficiency of different interventions was evaluated.
As shown in Figure 1, the SEIR model has four elements, which are S (susceptible), E (exposed, infected without infectivity), I (infected), and R (removed). The susceptible (S) who are infected by the infected (asymptomatic (IA), pre-symptomatic (PS), and symptomatic (IS)) become the exposed (E). According to whether symptoms appeared after infection, the exposed (E) is divided into the asymptomatic exposed (EA) and symptomatic exposed (ES). The asymptomatic exposed (EA) become the asymptomatic infected (IA) after 1/ε′ days, and then become the removed (RA) after 1/μ days. The symptomatic exposed (ES) become the pre-symptomatic infected (PS) after 1/ε days, and then become the symptomatic infected (IS) after 1/γ days. After the onset of symptoms, a proportion (α) of the symptomatic infected (IS) who preferred not to see a doctor become the removed (RS1) after 1/μ days. The other symptomatic infected (1-α) choose to be hospitalized (H) after 1/μ′ days and then become removed (RS2) after 1/μH days.
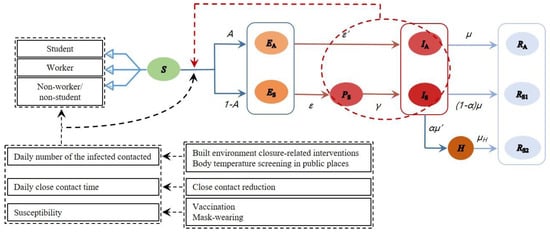
Figure 1.
The improved SEIR model considering both close contact behaviors and susceptibility.
In the simulation, the time step was set to 1 day. On the tth day after the appearance of the first confirmed case (IA and IS), the dynamics of COVID-19 transmission are listed in Equation (1) [11,23].
where A is the proportion of asymptomatic infected individuals among the infected; ε′ (day−1) is the rate from the asymptomatic exposed (EA) to the asymptomatic infected (IA); ε (day−1) is the rate from the symptomatic exposed (ES) to the pre-symptomatic infected (PS); γ (day−1) is the rate from the pre-symptomatic infected (PS) to the symptomatic infected (IS); α is the proportion of individuals who chose to be hospitalized during the symptomatic infection period (IS); μ′ (day−1) is the rate from the symptomatic infected (IS) to the hospitalized infected (H); μ (day−1) and μH (day−1) are the removal rate of the non-hospitalized infected (I) and the hospitalized infected (H), respectively; n(t) is the number of infected people contacted (PS, IA, and IS) per day, calculated by Equation (2); tp (h) is the daily close contact time per person, calculated by Equations (3) and (4).
where N is the population of a specific population group in Hong Kong; the subscripts S, W, and N represent students, workers, and non-workers/non-students, respectively; SP (%), WP (%), and NP (%) are the proportion of close contacts of students, workers, and non-workers/non-students, respectively and the values are shown in Figure S1 [24]; SP,I, WP,I, and NP,I are the infected population of students, workers, and non-workers/non-students, respectively; m is the daily number of closely contacted people of one population group.
where tin (h) is the total time spent indoors (exclude sleep time); CR (%) is the close contact rate (the ratio of the close contact time tC to the total time spent indoors tin).
Infection risk (ir) is the infection probability for the susceptible in close contact with an infected person per hour, and depends on the susceptibility of population groups and interventions (e.g., mask-wearing, vaccination). We conducted preliminary research on outbreaks in different cities/territories and assumed that the spread of the pandemic during the initial period (defined as the first 30 days from the start date when the cumulative number of confirmed cases exceeded 100) was regarded as the free spread without any intervention. The average monthly growth rate (defined as the ratio of cumulative confirmed cases on the 30th day to those on the first day) of six typical cities or territories was 73.1 (Table S1), and the ratio of susceptibility to COVID-19 of students, workers, and non-workers/non-students was 0.23:0.64:1 [25]. These were considered as the two prerequisites for choosing ir without any intervention.
2.2. Data Collection and Parameter Setting
As at the end of 2021, Hong Kong reported a total of 12.6 thousand confirmed cases since the first COVID-19 case was confirmed on 23 January 2020 [26]. The parameters involved in the model were divided into four categories (Table 1 and Table 2).
The first category was demographic data and close contact behavior-related parameters, including the proportion of the three population groups (student, worker, non-worker/non-student) and the real indoor close contact behaviors before the COVID-19 outbreak in Hong Kong. Students included the entire population aged 4–18 and the student population aged 19–24. Workers comprised the employed population aged 19–64 (not including the student population aged 19–24). Non-workers/non-students included babies aged 0–3 and elderly people over 65 years old. In Hong Kong, the numbers of students, workers, and non-workers/non-students were 1.1 million, 4.8 million, and 1.6 million, respectively (calculated according to Tables S2 and S3) and on average had close contacts with 20.8, 17.4, and 8.2 people per day (Table 1), with a total indoor close contact time of 8.3, 7.0, and 3.8 h per day (calculated according to Table 1 and Table S4) [27].
The second category was the initial setting of the population with different statuses (Table 2). The population in Hong Kong was assumed to be a constant of N. Among them, the initial values of IA and IS of students and non-worker/non-student were both equal to 0.
The third category was coefficients in the improved SEIR model (Table 2). Because the efficiency of different hospitalization rates on preventing the spread of COVID-19 was not significantly different (Figure S2), we assumed a median value for the hospitalization rate.
The fourth category was intervention-related data on the mask filtration efficiency, CoronaVac COVID vaccine (Sinovac) efficiency, probability of fever in the COVID-19 infected, correctness of body temperature screening in public places, and sensitivity of NAT (Table 2).

Table 1.
Demographic data and close contact behavior-related parameters before the COVID-19 outbreak in Hong Kong.
Table 1.
Demographic data and close contact behavior-related parameters before the COVID-19 outbreak in Hong Kong.
| Type | Parameters | Value | Ref. | ||
|---|---|---|---|---|---|
| Student | Worker | Non-Worker/Non-Student | |||
| Population distribution | 14.6% | 63.5% | 21.9% | [28] | |
| Daily number of closely contacted people (m) | School | 8.3 | - | - | [27] |
| Workplace | - | 7.5 | - | ||
| Supermarket | 1.5 | 2.1 | 2.1 | ||
| Public transport | 2.5 | 2.5 | 1.5 | ||
| Shopping center | 2.0 | 1.9 | 2.6 | ||
| Restaurant | 3.4 | 1.7 | 1.1 | ||
| Home | 3.2 | 1.7 | 0.8 | ||
| Close contact rate 1 (CR, %) | School | 64 | - | - | [27] |
| Workplace | - | 55 | - | ||
| Supermarket | 28 | 26 | 22 | ||
| Public transport | 32 | 25 | 17 | ||
| Shopping center | 37 | 17 | 19 | ||
| Restaurant | 47 | 39 | 29 | ||
| Home | 62 | 57 | 31 | ||
1 Close contact rate in this study was based on the daily close contact time before the outbreak in Hong Kong.

Table 2.
Simulation-related parameters of the improved SEIR model.
Table 2.
Simulation-related parameters of the improved SEIR model.
| Type | Parameters | Value | Ref. |
|---|---|---|---|
| The initial setting of the population with different statuses | N | 7,500,000 | [8] |
| S(0) | 7,499,999 | Assumed | |
| E(0) | 0 | Assumed | |
| I(0) | 1 (IA = 0.25; Is = 0.75) | Assumed | |
| R(0) | 0 | Assumed | |
| Coefficients in the improved SEIR model | A | 1/4 | [29] |
| 1/3 | [30] | ||
| 1/5 | [30] | ||
| 1/2 | [30] | ||
| 45.0% | Assumed 1 | ||
| 2/5 | [22] | ||
| 1/2 | Assumed 2 | ||
| 1/8 | [31] | ||
| Intervention-related data | Mask filtration efficiency 3 | 64.3% | [32] |
| Vaccine effectiveness 4 | 67.0% | [33] | |
| Probability of fever in the infected | 46.7% | [34] | |
| Correctness of body temperature screening | 86.0% | [13] | |
| Sensitivity of NAT 5 | 84.8% | [35] |
1 Hospitalization rate: 90% of symptomatic individuals (IS) were assumed to see a doctor and 50% of these people were assumed to go to the hospital for treatment, so the hospitalization rate was set to 45% (90% × 50%) (Figure S2). 2 Assuming that the proportion (1 − α) of the symptomatic infected (IS) would spend 2 days for hospitalization (H) after symptom onset. 3 Mask-wearing reduced 64.3% of viral load. When both the infected (IA, PS, and IS) and the susceptible (S) wore masks simultaneously, the infection risk ir would decrease by 87.3% (1 − (1 − 64.3%) × (1 − 64.3%)). 4 The proportion of people who would not be infected after being vaccinated (assuming all residents vaccinating the CoronaVac COVID vaccine (Sinovac) [36]). This study used the average value of the Sinovac vaccine’s effectiveness. 5 Nasopharyngeal swab was used as the sampling site.
2.3. Model Scenarios
2.3.1. Parameter Setting
When implementing built environment closure-related interventions, the number of close contacts should be calculated considering both the total number of contacts before the pandemic and the number of contacts in the corresponding environment.
When school closures, workplace closures, and stay-at-home orders for non-worker/ non-student interventions were implemented, the proportion of contacts during the COVID-19 pandemic was determined. When implementing other interventions, the proportion of contacts before the COVID-19 pandemic was determined.
2.3.2. Case Study
The effectiveness of six types of interventions (built environment closure-related interventions, mask-wearing, vaccination, close contact reduction, nucleic acid testing, body temperature screening in public places) in terms of implementation time (31th, 61th, 91th day) and intensity (0, 25%, 50%, 75%, 100%) was evaluated using Python. Taking COVID-19 spread without any interventions as an example, the relevant code is shown in Section S2.
The built environment included schools, workplaces, homes, supermarkets, public transport, shopping centers, and restaurants in this study. Assuming that the supermarkets were always open during the COVID-19 pandemic, built environment closure-related interventions only considered the other six built environments.
When evaluating the time to implement interventions, the implementation intensity was set to 100%. When evaluating the intensity, it was assumed that the interventions would be implemented 30 days after the first confirmed COVID-19 case appeared. All scenarios were simulated for 500 days.
3. Results
3.1. Basic Results
Considering both real human close contact behaviors and susceptibility of different population groups, the infection risk of COVID-19 of students, workers, and non-workers/non-students was 3.1%, 8.7%, and 13.6%, respectively. Without any intervention, at 1 month after the first confirmed COVID-19 case in Hong Kong, 0.01% of residents would be infected. Four months later, the number of the infected reached its peak. After roughly eight months, the spread of the pandemic gradually disappeared, and about 5.9 million people (79.3%) were eventually infected (Figure 2).
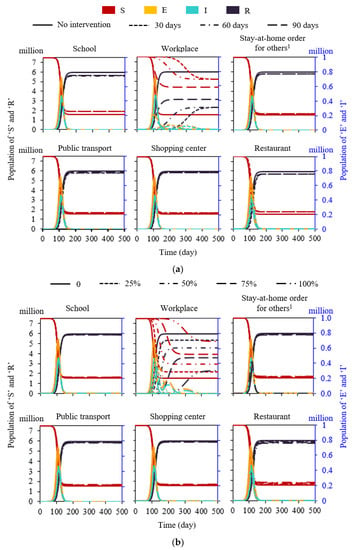
Figure 2.
Efficiency of typical built environment closure-related interventions. (a) Implementation time (proportion was assumed to be 100%). (b) Implementation intensity (interventions were assumed to be implemented on the 31th day after the first confirmed case). 1 Non-workers/non-students.
3.2. Built Environment Closure-Related Interventions
When five single built environment closure-related interventions (school closures, stay-at-home orders for non-workers/non-students, public transport closures, shopping center closures, and restaurant closures) were implemented on the 31th, 61th, and 91th day after the first COVID-19 confirmed case appeared, the time to implement interventions had no significant impact on the final total infections. In addition, these five interventions contributed little to restraining the COVID-19 outbreak. Compared with no intervention, the final infection rate decreased by 5.6% (school closures), 4.3% (restaurant closures), 2.5% (stay-at-home orders for non-workers/non-students), 2.3% (public transport closures), and 1.9% (shopping center closures), respectively (Figure 2a). When all workplaces were closed on the 31th, 61th, and 91th day after the first COVID-19 confirmed case appeared, there was no significant impact on the final infections and the total infections decreased by 56.8% on average compared with no intervention (Figure 2a).
The impact of the proportions (0, 25%, 50%, 75%, 100%) of class suspension, work suspension, stay-at-home orders for non-workers/non-students, public transport closures, shopping center closures, and restaurant closures on the COVID-19 prevention and control are shown in Figure 2b. When the proportion of work suspension was 25%, 50%, 75%, and 100%, respectively, the infection rate dropped by 10.6%, 23.5%, 39.8%, and 61.5%, respectively (Figure 2b).
When the proportion of both work and class suspensions was 25%, 50%, 75%, and 100%, the infection rate dropped by 14.3%, 29.1%, 47.4%, and 73.6%, respectively (Figure S3). When the proportion of work and class suspensions and stay-at-home orders for non-workers/non-students was 25%, 50%, 75%, and 100%, the infection rate dropped by 13.8%, 30.5%, 53.1%, and 99.5%, respectively (Figure S3). Comparing these three interventions related to workplace closures, we found that workplace closures contributed at least 62% to reducing the COVID-19 infections (Figure S3). Workplace closures were more effective for pandemic control among six built environment closure-related interventions.
Figure 3a shows the absolute infection rate of the three population groups (student, worker, and non-worker/non-student) among the COVID-19 infections in Hong Kong. When the school closures were implemented, the absolute infection rate of students was the lowest (3.5%) in all built environment interventions. When the workplace closures were implemented, the absolute infection rate of workers was the lowest (53.9%). When stay-at-home orders for non-workers/non-students were implemented, the absolute infection rate of non-workers/non-students was the lowest (21%).
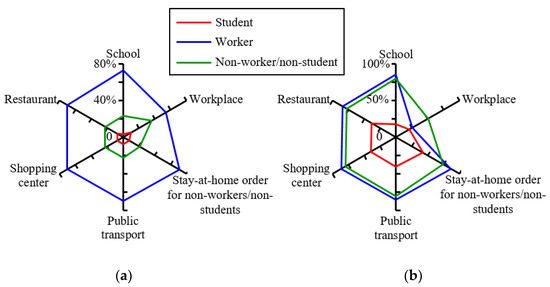
Figure 3.
Infection rate under typical built environment-closure interventions (interventions were assumed to be implemented on the 31th day after the first confirmed case). (a) Absolute infection rate (the ratio of the total infections of students, workers, and non-workers/non-students to the total infections). (b) Relative infection rate (the ratio of the total infections of students, workers, and non-workers/non-students to the total number of students, workers, and non-workers/non-students, respectively).
For the interventions mentioned above, the relative infection rates of students, workers, and non-workers/non-students ranged from 18.0% to 42.1%, 25.9% to 86.5%, and 50.5% to 80.5%, respectively (Figure 3b). When school closures were implemented, the relative infection rate of students was the lowest and decreased by 57.6% compared with no intervention. However, the relative infection rate of non-workers/non-students was the highest (80.5%, decreased by 1.6% compared with no intervention), and was 4.8 times that of students and 0.9 times that of workers. When workplace closures were implemented, the relative infection rate of workers and non-workers/non-students was the lowest and decreased by 70.2%, and 38.3% compared with no intervention. When stay-at-home orders for non-workers/non-students were implemented, the relative infection rate of students and workers was the highest, 42.1% (decreased by 1.0% compared with no intervention) and 86.5% (decreased by 0.5% compared with no intervention), respectively. Overall, when workplace closures were implemented, the infection rate of the total population in Hong Kong was the lowest (30.6%), and decreased by 61.4% compared with no intervention.
3.3. Mask-Wearing
Due to the fact that people did not often wear masks at homes and in restaurants [11], this study only considered two scenarios: only in shopping centers, supermarkets, and public transport; and in all built environments except homes and restaurants (Figure 4). When only wearing masks in shopping centers, supermarkets, and public transport, 5.9 million (74.9%) people would be infected with the SARS-CoV-2, reduced by 5.5% compared with no intervention (Figure 4a). The time and the proportion of implementing interventions had no significant impact on restraining the spread of COVID-19. However, if the mask-wearing could be mandatorily implemented in all built environments except homes and restaurants on the 31th, 61th, and 91th day after the appearance of the first confirmed COVID-19 case, the total number of infections (rate) would be 0.8 million (10.3%), 1.3 million (16.7%), and 2.5 million (33.5%), respectively, and decreased by 87.0%, 78.9%, and 57.7% compared with no intervention (Figure 4a). Assuming that the proportion of the mask-wearing population was 25%, 50%, and 75% in schools, workplaces, shopping centers, and public transports, the total infections would be decreased by 12.7%, 28.4%, and 49.5% compared with no intervention (Figure 4b).
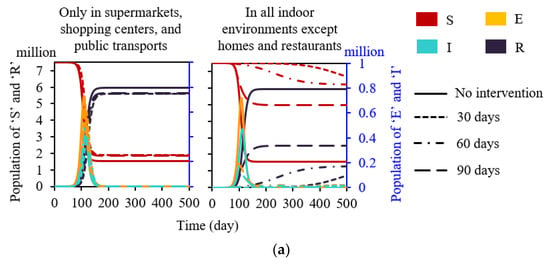
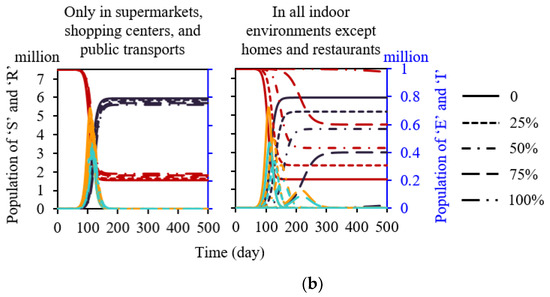
Figure 4.
Efficiency of the mask-wearing in built environments under two scenarios (only in shopping centers and public transport; in all built environments except homes and restaurants). (a) Implementation time (proportion was assumed to be 100%). (b) Implementation intensity (interventions were assumed to be implemented on the 31th day after the first confirmed case).
3.4. Vaccination
The total infections would be reduced by 99.99%, 99.6%, and 83.8% compared with no intervention if all residents were vaccinated on the 31th, 61th, and 91th day after the first infected case appeared. (Figure 5a). Workers should be prioritized for vaccination, followed by non-workers/non-students and students. If only 1 million people were vaccinated under the order of workers, random, non-workers/non-students, and students, the total infections would be reduced by 0.95 million (16.0%), 0.85 million (14.3%), 0.73 million (12.3%), and 0.43 million (7.3%), respectively, compared with no intervention (Figure 5b). Under the order of vaccination, when the vaccination rate was 60%, the total infections decreased the most, reaching 1.7 million, compared with random vaccination (Figure 5c).
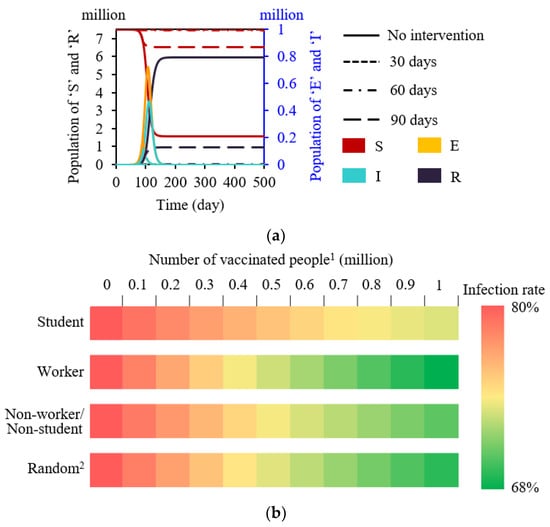
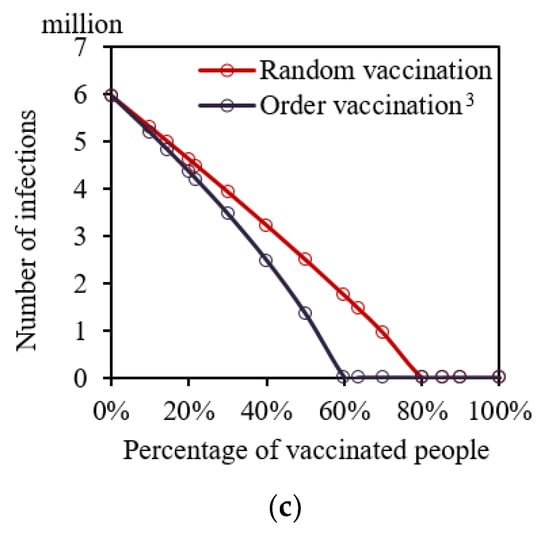
Figure 5.
Vaccination strategy analysis. (a) Implementation time (assuming the proportion of vaccination was 100%). (b) Priority strategy for vaccination for three population groups if only 1 million people are vaccinated (interventions were assumed to be implemented on the 30th day after the first confirmed case). (c) Vaccination order if all residents (7.5 million) are vaccinated. 1 People who had successfully injected all vaccine doses. 2 Persons in each population group had the same probability to be vaccinated. When 1 million residents are vaccinated, the ratios of students, workers, and non-students/non-workers to be vaccinated are 14.6%:63.5%:21.9%, respectively. 3 Workers were prioritized to be vaccinated, followed by non-workers/non-students and students.
3.5. Other Single Interventions
As shown in Figure 6, performing NAT when the number of confirmed COVID-19 cases in Hong Kong (Figure 6a) reached a particular proportion was better than performing NAT with a constant time interval (Figure S4). In total, 34 implementations of NAT would be undertaken within 500 days if performing NAT when the number of confirmed cases reached 0.01% of the total population. The number of final total infections was 0.1 million (1.6%), which decreased by 98.0% compared with no intervention (Figure 6a). Body temperature screening in public places can filter out some infected people with fever. Correctness of body temperature screening in public places had a significant impact on the infection spread (Figure 6b), but implementation time did not (Figure S5). When the correctness of body temperature screening in public places was 25% and 100%, the total infections were decreased by 9.9% and 36.5%, respectively, compared with no intervention (Figure 6b). Social distancing could reduce the spread of the COVID-19. If the daily close contact reduction rate was 50%, the infection rate would decrease to 13.5% and would be decreased by 83.0% compared with any intervention (Figure 6c).
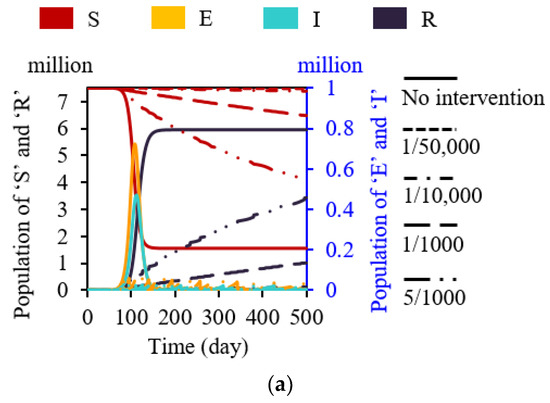
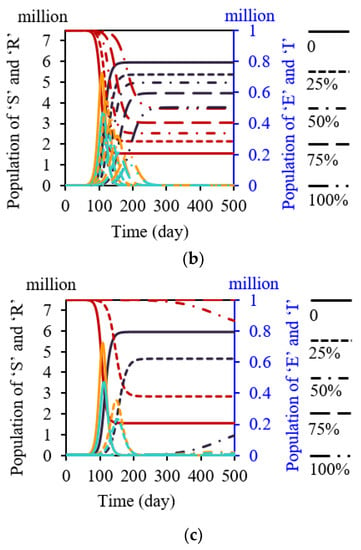
Figure 6.
Effectiveness of the time and proportions of other intervention implementations. (a) All residents would perform NAT 1 when the number of infected exceeded a certain proportion). (b) Correctness of body temperature screening in public places 2. (c) Close contact reduction rate (based on the daily close contact time of residents before the COVID-19 pandemic in Hong Kong). 1 Sensitivity of NAT was 84.8%. 2 Public places including schools, workplaces, supermarkets, public transport, shopping centers, and restaurants.
3.6. Combined Interventions
Taking two relatively more efficient interventions of built environment closure-related intervention (workplace and school closures), we analyzed the pairwise combination of interventions of school closures (Figure 7a), workplace closures (Figure 7b), vaccination (Figure 7c), mask-wearing (Figure 7d), close contact reduction (Figure 7e), and body temperature screening in public places (Figure 7f). Close contact reduction was the best intervention, followed by vaccination, mask-wearing, workplace closures, body temperature screening in public places, and school closures. When the close contact reduction rate was 59.9% or the vaccination rate reached 89.5%, the basic reproduction number R0 was equal to 1, which meant the pandemic would not break out. The other four single interventions cannot achieve a R0 value smaller than 1. The effect of the combined interventions of mask-wearing and body temperature screening in public places was better than the combination of mask-wearing and workplace closures. Regardless of the combination of mask-wearing and body temperature screening in public places with school closures or workplace closures, the COVID-19 would not be controlled.
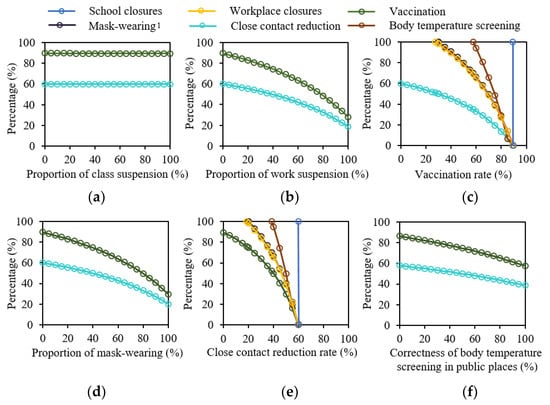
Figure 7.
Effectiveness of the combination of two interventions. (a) School closures. (b) Workplace closures. (c) Vaccination. (d) Mask-wearing. (e) Close contact reduction. (f) Body temperature screening in public places. 1 Wearing masks was in schools, workplaces, supermarkets, shopping centers, and public transports.
4. Discussion
The COVID-19 pandemic has lasted for nearly two years since the first confirmed case appeared. The total infections dropped significantly when all interventions were implemented simultaneously. The choice of implementation of interventions to minimize the interference on society and human lives was very important. This study established an improved SEIR model considering both real indoor close contact behaviors and personal susceptibility of three population groups (student, worker, non-worker/non-student). Taking Hong Kong as an example, the effectiveness of the time (31th, 61th, 91th day) and intensity (0, 25%, 50%, 75%, 100%) of implementation of the single and combined interventions, including built environment closure-related interventions, mask-wearing, vaccination, close contact reduction, NAT, and body temperature screening in public places, was analyzed.
4.1. Built Environment Closure-Related Interventions
Students and workers spent a lot of time and had the highest daily number of close contacts in schools and workplaces [27]. Consistent with the previous studies [37,38], we also found workplace closures were more effective among six typical built environment closure-related interventions. Because of relatively high susceptibility (2.8 times higher than students, [25]) and large population (63.5% of the total population in Hong Kong, [39]), the total number of infections decreased by 61.4% compared with no intervention. Therefore, teleworking at home, staggered shifts, and extending holidays were common interventions for the COVID-19 pandemic [40].
School closures were significant in restraining the spread of influenza [41]. However, students had a relatively lower susceptibility to COVID-19, and the number of students in Hong Kong was relatively small (14.6% of the total population). Therefore, the total COVID-19 infections only decreased by 5.6% due to implementing school closures compared with no intervention. School closures had little impact on the spread of COVID-19, preventing 2~4% of deaths [42,43]. Considering the mechanisms on COVID-19 transmission was not clear at the beginning of the pandemic, many high school and college students adopted the strategy of online learning to mitigate the stress of the COVID-19 pandemic in many countries [40].
Stay-at-home orders for non-workers/non-students would not be effective in reducing the total infections. Non-workers/non-students spent 3.5 h in close contact with others at home every day on average (exclude sleep time). Relevant data showed that during the COVID-19 pandemic, the close contact reduction rate in the family decreased by only 8.3% [27]. In China, the COVID-19 infection risk of household contacts was 10 times that of other countries [44], and more than 65% of COVID-19 infections were infected at home [11,45]. However, based on the assumption that short-range transmission was the main transmission route, there were few measures to reduce family infections at present.
4.2. Other Single Interventions
During the COVID-19 pandemic, in addition to built environment closure-related interventions, other interventions were also implemented, such as mask-wearing, vaccination, NAT, close contact reduction, and body temperature screening in public places.
Mask-wearing was widely used to restrain the infection risk of COVID-19 spread through close contact because it can effectively decrease the aerosols both exhaled by the infected and inhaled by the susceptible [46]. On April 6th, 2020, the World Health Organization suggested the use of masks [47]. From April 6th to May 9th, 2020, the total number of infections was reduced by 78,000 only by mask-wearing in Italy, while reduced by 66,000 from 17 April to 9 May in New York [48]. Due to the fact that people seldom wore masks at homes and in restaurants [11], we only analyzed the mask-wearing in other built environments. If mask-wearing was only mandatorily required (implementation intensity was 100%) in shopping centers, supermarkets, and public transport, the effect was the same as when the mask-wearing proportion was 12.0% in all built environments including schools, workplaces, supermarkets, shopping centers, and public transports.
Vaccination strategies directly affected the infection risk [49,50]. Considering the difference in susceptibility, we found that workers were a higher priority for vaccination, followed by non-workers/non-students and students. This was mainly due to the relatively high susceptibility and large population of workers in the study. However, the Joint Committee on Vaccination and Immunization recommended that the population over the age of 65 be given priority for vaccination [51] considering their lower immunity and higher mortality [52]. In addition, one study [14] suggested that students should be prioritized for vaccination because the difference in the susceptibility for various population groups was ignored.
Studies showed that timely NAT was one of the most effective interventions [53]. We found that when the number of infected reached 0.01% of the total population, the infection rate could be effectively controlled at 1.6% by organizing all residents to perform NAT. However, NAT would cause a lot of resource waste and environmental pollution.
Before the outbreak in Hong Kong, students, workers, and non-workers/non-students, respectively, spent 58%, 46%, and 29% of their daily time in indoor close contact [27]. Social distancing would reduce the infection risk of COVID-19. We found when the close contact reduction rate was at least 59.9%, the pandemic was within a controllable range in Hong Kong. When the close contact reduction rate was 50%, the infections would be reduced by 83.0%. However, when considering overseas import cases, the infections can be reduced by 70% [11]. Body temperature screening can quickly identify people with fever and reduce the infection risk of susceptible people in public areas. Considering that 31–55% of COVID-19 infections had no fever symptoms [34,54] and limited correctness of temperature detectors [13], the effectiveness of body temperature screening was low. We found that even if the correctness of body temperature screening reached 100%, the infection rate was only reduced by 36.5% compared with no intervention, and this was consistent with previous studies [11]. Therefore, body temperature screening in public places should be implemented with other interventions.
4.3. Combined Interventions
It is challenge for a single intervention to effectively control the spread of the COVID-19 pandemic. Therefore, the effectiveness of combined interventions should be analyzed to support strategy making. Close contact reduction was a better intervention, followed by vaccination, mask-wearing, workplace closures, body temperature screening in public places, and school closures. Close contact reduction and vaccination were the best two interventions; either of these measures can effectively control the spread of COVID-19 if strictly implemented. The other four measures should be implemented in conjunction with other interventions to achieve the effect of control. Although workplace closures were more effective than body temperature screening in public places, the latter had higher efficacy combined with mask-wearing than the former. Because mask-wearing in workplaces would significantly reduce the COVID-19 infections, the infection risk reduction was limited when both mask-wearing and workplace closures were implemented simultaneously.
In the early stage of the outbreak in Hong Kong, close contact reduction was popularly used to restrain the development of the pandemic, consistent with the World Health Organization’s recommendation to maintain a social distance of at least 1 m in public places [55]. Close contact reduction and wearing masks have typically been a common combination of interventions [56]. However, close contact reduction was determined by personal preference and was difficult to be controlled mandatorily. Therefore, encouraging the public to be vaccinated and wearing masks was an easy-to-implement and relatively safe combination intervention. However, the vaccination rate in Hong Kong was only 34.3% in August 2021 [57], which meant that at least 96% of residents need to wear masks for COVID-19 control in our study. When the vaccination rate increased to 50% and 75%, the proportion of mask-wearing could be no less than 79.6% and 39.1%, respectively, to achieve an R0 smaller than 1. However, many residents have stopped wearing masks due to vaccination. Therefore, in August 2021, while encouraging residents to be vaccinated, the Chinese government has implemented new requirements for residents to wear masks [58]. The World Health Organization encouraged people to keep their distance, wear masks, and be vaccinated simultaneously [59]. Body temperature screening was popular in public places, but was not effective in mitigating outbreaks. When the correctness of temperature screening in all public places stabilized at 86% [16], even if the proportion of wearing masks was 100%, the pandemic cannot be controlled.
However, this study has some limitations. First, we only considered the impact of close contact behaviors on the spread of the COVID-19 pandemic, ignoring the effect of long-range airborne, surface, and fecal–oral transmission [3,4,6]. Second, our model did not consider the influence of environmental temperature [60], humidity [61], and climate change [62] on virus activity. In addition, we did not take close contact behavior of more population groups into account. For example, the close contact behavior (number, duration, and proportion) of children and adolescents included in ‘students’ in our study and the proportion of contact with population groups in different public places were different [63,64]. Finally, the efficiency of vaccination was different for population groups [65], which was ignored in the study. In future research, more influencing factors and interventions should be considered to improve the accuracy and reliability of the simulation.
5. Conclusions
In order to evaluate the efficiency of different interventions, this study established an improved SEIR model considering both real indoor close contact behaviors and susceptibility of three population groups (student, worker, and non-worker/non-student). Taking Hong Kong as an example, the effectiveness of single and combined interventions was analyzed, and the main findings were:
- The infection risk (one-hour close contact with an infected person) of students, workers, and non-students/workers was 3.1%, 8.7%, and 13.6%, respectively.
- Workplace closures were more effective for COVID-19 control among built environment closure-related interventions, on average reducing total infections by 56.8% compared with no intervention.
- Mask-wearing in workplaces and schools was much more effective than in shopping centers and public transport.
- Workers should be prioritized for vaccination, followed by non-workers/non-students and students.
- Close contact reduction was a better intervention, followed by vaccination, mask-wearing, workplace closures, body temperature screening in public places, school closures, restaurant closures, stay-at-home orders for non-workers/non-students, public transport closures, and shopping center closures.
- When the close contact reduction rate was 59.9% or the vaccination rate reached 89.5%, R0 was equal to 1, which was the critical point at which the COVID-19 pandemic would not break out.
The results of this study may provide scientific support for the government to implement strategies for pandemic prevention and control of COVID-19 transmission.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/buildings12030365/s1. Supplementary Materials have two parts, Sections S1 and S2. Table S1: The monthly growth rate of confirmed cases at the initial period of the COVID-19 outbreak in different cities/territories; Table S2: The proportion of the population by age in Hong Kong; Table S3: Percentage of the three population groups (student, worker, non-worker/non-student) in Hong Kong; Table S4: Daily time spent (exclude sleep time) indoors of three population groups (student, worker, non-worker/non-student) in public places before the outbreak of COVID-19 in Hong Kong; Figure S1: Proportion of contacts between three population groups before the outbreak and during the outbreak; Figure S2: Effects of different hospitalization rates on the efficiency of COVID-19 prevention and control; Figure S3: Effectiveness of the proportion of both work and class suspension and the proportion of work and class suspension and stay-at-home orders for non-workers/students implementations; Figure S4: Effectiveness of the time to implement NAT; Figure S5: Efficiency of the time to implement body temperature screening in public places; The relevant code of the Python program for no pandemic interventions is shown in Section S2.
Author Contributions
Conceptualization, N.Z.; methodology, D.M. and N.Z.; validation, D.M.; formal analysis, D.M.; investigation, D.M.; resources, N.Z.; data curation, D.M.; writing—original draft preparation, D.M.; writing—review and editing, D.M. and N.Z.; visualization, D.M. and N.Z.; supervision, N.Z.; project administration, N.Z.; funding acquisition, N.Z. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by the Natural Science Foundation of China, grant number 52108067.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The original details of the data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Coronavirus (COVID-19) Dashboard: Situation by Region, Country Territory Area, World Health Organization. Available online: https://covid19.who.int/table/ (accessed on 29 January 2022).
- OECD. Global Outlook on Financing for Sustainable Development 2021; Organisation for Economic Co-operation and Development: Paris, France, 2020. [Google Scholar]
- Law, R.; Lai, J.; Edwards, D.J.; Hou, H.Y. COVID-19: Research Directions for Non-Clinical Aerosol-Generating Facilities in the Built Environment. Buildings 2021, 11, 282. [Google Scholar] [CrossRef]
- Wan, J.Y.; Wei, J.J.; Lin, Y.T.; Zhang, T.F. Numerical Investigation of Bioaerosol Transport in a Compact Lavatory. Buildings 2021, 11, 526. [Google Scholar] [CrossRef]
- Chen, W.; Zhang, N.; Wei, J.; Yen, H.; Li, Y. Short-range airborne route dominates exposure of respiratory infection during close contact. Build. Environ. 2020, 176, 106859. [Google Scholar] [CrossRef]
- Zhai, Z.Q.; Li, H.; Bahl, R.; Trace, K. Application of Portable Air Purifiers for Mitigating COVID-19 in Large Public Spaces. Buildings 2021, 11, 329. [Google Scholar] [CrossRef]
- Qian, H.; Miao, T.; Liu, L.; Zheng, X.; Luo, D.; Li, Y. Indoor transmission of SARS-CoV-2. Indoor Air 2021, 31, 639–645. [Google Scholar] [CrossRef]
- Yamey, G.; Walensky, R.P. COVID-19: Re-opening universities is high risk. BMJ 2020, 370, 3365. [Google Scholar] [CrossRef]
- Zhang, N.; Chen, X.; Jia, W.; Jin, T.; Xiao, S.; Chen, W.; Hang, J.; Ou, C.; Lei, H.; Qian, H.; et al. Evidence for lack of transmission by close contact and surface touch in a restaurant outbreak of COVID-19. J. Infect. 2021, 83, 207–216. [Google Scholar] [CrossRef]
- Wu, W.S.; Li, Y.G.; Wei, Z.F.; Zhou, P.H.; Lyu, L.K.; Zhang, G.P.; Zhao, Y.; He, H.Y.; Li, X.Y.; Gao, L.; et al. Investigation and analysis on characteristics of a cluster of COVID-19 associated with exposure in a department store in Tianjin. Chin. J. Epidemiol. 2020, 41, 489–493. [Google Scholar]
- Zhang, N.; Chan, P.-T.J.; Jia, W.; Dung, C.-H.; Zhao, P.; Lei, H.; Su, B.; Xue, P.; Zhang, W.; Xie, J.; et al. Analysis of efficacy of intervention strategies for COVID-19 transmission: A case study of Hong Kong. Environ. Int. 2021, 156, 106723. [Google Scholar] [CrossRef]
- Chen, Y.; Fang, C. Combined interventions to suppress R0 and border quarantine to contain COVID-19 in Taiwan. J. Formos. Med. Assoc. 2021, 120, 903–905. [Google Scholar] [CrossRef]
- Koo, J.R.; Cook, A.R.; Park, M.; Sun, Y.; Sun, H.; Lim, J.T.; Tam, C.; Dickens, B.L. Interventions to mitigate early spread of SARS-CoV-2 in Singapore: A modelling study. Lancet Infect. Dis. 2020, 20, 678–688. [Google Scholar] [CrossRef] [Green Version]
- Mendez-Brito, A.; El, B.C.; Pozo-Martin, F. Systematic review of empirical studies comparing the effectiveness of non-pharmaceutical interventions against COVID-19. J. Infect. 2021, 83, 281–293. [Google Scholar] [CrossRef] [PubMed]
- Pozo-Martin, F.; Weishaar, H.; Cristea, F.; Hanefeld, J.; Bahr, T.; Schaade, L.; El Bcheraoui, C. The impact of non-pharmaceutical interventions on COVID-19 epidemic growth in the 37 OECD member states. Eur. J. Epidemiol. 2021, 36, 629–640. [Google Scholar]
- Quilty, B.J.; Clifford, S.; Flasche, S.; Eggo, R.M.; Cmmid, N.W.G.; Cmmid, N.W.G. Effectiveness of airport screening at detecting travellers infected with novel coronavirus (2019-nCoV). Eurosurveillance 2020, 25, 1. [Google Scholar] [CrossRef] [PubMed]
- Olanrewaju, A.; Abdulaziz, A.; Preece, C.N.; Shobowale, K. Evaluation of measures to prevent the spread of COVID-19 on the construction sites. Clean. Eng. Technol. 2021, 5, 100277. [Google Scholar] [CrossRef]
- China Encourages Voluntary COVID-19 Vaccination: Official. Available online: http://en.people.cn/n3/2021/0410/c90000-9837712.html (accessed on 29 January 2022).
- Iran Allocates Funds to Import COVID-19 Vaccines; Kuwait Starts National Vaccination Campaign. Available online: http://en.people.cn/n3/2020/1225/c90000-9802937.html (accessed on 29 January 2022).
- How COVID-19 Has Impacted Global Construction Markets—RLB|Asia. 2022. Available online: https://www.rlb.com/asia/insight/how-covid-19-has-impacted-global-construction-markets/ (accessed on 29 January 2022).
- Ihme, C.F.T. Modeling COVID-19 scenarios for the United States. Nat. Med. 2021, 27, 94–105. [Google Scholar]
- Aleta, A.; Martín-Corral, D.; Piontti, A.P.; Ajelli, M.; Litvinova, M.; Chinazzi, M.; Dean, N.E.; Halloran, M.E.; Longini, I.M., Jr.; Merler, S.; et al. Modelling the impact of testing, contact tracing and household quarantine on second waves of COVID-19. Nat. Hum. Behav. 2020, 4, 964–971. [Google Scholar] [CrossRef]
- Yang, Z.; Zeng, Z.; Wang, K.; Wong, S.-S.; Liang, W.; Zanin, M.; Liu, P.; Cao, X.; Gao, Z.; Mai, Z.; et al. Modified SEIR and AI prediction of the epidemics trend of COVID-19 in China under public health interventions. J. Thorac. Dis. 2020, 12, 165–174. [Google Scholar] [CrossRef]
- Zhang, J.; Litvinova, M.; Liang, Y.; Wang, Y.; Wang, W.; Zhao, S.; Wu, Q.; Merler, S.; Viboud, C.; Vespignani, A.; et al. Changes in contact patterns shape the dynamics of the COVID-19 outbreak in China. Science 2020, 368, 1481–1486. [Google Scholar] [CrossRef]
- Jing, Q.-L.; Liu, M.-J.; Zhang, Z.-B.; Fang, L.-Q.; Yuan, J.; Zhang, A.-R.; E Dean, N.; Luo, L.; Ma, M.-M.; Longini, I.; et al. Household secondary attack rate of COVID-19 and associated determinants in Guangzhou, China: A retrospective cohort study. Lancet Infect. Dis. 2020, 20, 1141–1150. [Google Scholar] [CrossRef]
- GOV.HK. COVID-19 Thematic Website—Together, We Fight the Virus—Home. Available online: https://www.coronavirus.gov.hk/eng/index.html#Updates_on_COVID-19_Situation (accessed on 29 January 2022).
- Zhang, N.; Jia, W.; Lei, H.; Wang, P.; Zhao, P.; Guo, Y.; Dung, C.-H.; Bu, Z.; Xue, P.; Xie, J.; et al. Effects of human behaviour changes during the COVID-19 pandemic on influenza spread in Hong Kong. Clin. Infect. Dis. 2021, 73, 1142–1150. [Google Scholar] [CrossRef] [PubMed]
- Snapshot of Hong Kong. Available online: https://www.censtatd.gov.hk/en/scode460.html (accessed on 29 January 2022).
- Nishiura, H.; Kobayashi, T.; Miyama, T.; Suzuki, A.; Jung, S.-M.; Hayashi, K.; Kinoshita, R.; Yang, Y.; Yuan, B.; Akhmetzhanov, A.R.; et al. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19). Int. J. Infect. Dis. 2020, 94, 154–155. [Google Scholar] [CrossRef] [PubMed]
- Backer, J.A.; Klinkenberg, D.; Wallinga, J. Incubation period of 2019 novel coronavirus (2019-nCoV) infections among travellers from Wuhan, China, 20–28 January 2020. Eurosurveillance 2020, 25, 2000062. [Google Scholar] [CrossRef] [Green Version]
- Verity, R.; Okell, L.C.; Dorigatti, I.; Winskill, P.; Whittaker, C.; Imai, N.; Cuomo-Dannenburg, G.; Thompson, H.; Walker, P.G.T.; Fu, H.; et al. Estimates of the severity of coronavirus disease 2019: A model-based analysis. Lancet Infect. Dis. 2020, 20, 669–677. [Google Scholar] [CrossRef]
- Milton, D.K.; Fabian, M.P.; Cowling, B.J.; Grantham, M.L.; Mcdevitt, J.J. Influenza virus aerosols in human exhaled breath: Particle size, culturability, and effect of surgical masks. PLoS Pathog. 2013, 9, e1003205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Why Is There a Big Difference in Phase Three of Sinovac Vaccine? Available online: https://baijiahao.baidu.com/s?id=1693342268153415934&wfr=spider&for=pc (accessed on 29 January 2022).
- Buckner, F.S.; McCulloch, D.J.; Atluri, V.; Blain, M.; A McGuffin, S.; Nalla, A.K.; Huang, M.-L.; Greninger, A.L.; Jerome, K.R.; A Cohen, S.; et al. Clinical Features and Outcomes of 105 Hospitalized Patients With COVID-19 in Seattle, Washington. Clin. Infect. Dis. 2020, 71, 2167–2173. [Google Scholar] [CrossRef] [PubMed]
- Butler-Laporte, G.; Lawandi, A.; Schiller, I.; Yao, M.; Dendukuri, N.; McDonald, E.G.; Lee, T.C. Comparison of Saliva and Nasopharyngeal Swab Nucleic Acid Amplification Testing for Detection of SARS-CoV-2. JAMA Intern. Med. 2021, 181, 353. [Google Scholar] [CrossRef] [PubMed]
- GOV.HK. About the Vaccines. Available online: https://www.covidvaccine.gov.hk/en/vaccine (accessed on 29 January 2022).
- Dreher, N.; Spiera, Z.; Mcauley, F.M.; Kuohn, L.; Durbin, J.R.; Marayati, N.F.; Ali, M.; Li, A.Y.; Hannah, T.C.; Gometz, A.; et al. Policy Interventions, Social Distancing, and SARS-CoV-2 Transmission in the United States: A Retrospective State-level Analysis. Am. J. Med. Sci. 2021, 361, 575–584. [Google Scholar] [CrossRef] [PubMed]
- Wibbens, P.D.; Koo, W.W.; Mcgahan, A.M. Which COVID policies are most effective? A Bayesian analysis of COVID-19 by jurisdiction. PLoS ONE 2020, 15, e244177. [Google Scholar] [CrossRef]
- Population Estimates. Available online: https://www.censtatd.gov.hk/en/scode150.html (accessed on 29 January 2022).
- Fong, M.W.; Gao, H.; Wong, J.Y.; Xiao, J.; Shiu, E.Y.; Ryu, S.; Cowling, B.J. Nonpharmaceutical Measures for Pandemic Influenza in Nonhealthcare Settings—Social Distancing Measures. Emerg. Infect. Dis. 2020, 26, 976. [Google Scholar] [CrossRef]
- Rebmann, T.; Elliott, M.; Swick, Z.; Reddick, D. US School Morbidity and Mortality, Mandatory Vaccination, Institution Closure, and Interventions Implemented During the 2009 Influenza A H1N1 Pandemic. Biosecur. Bioterror. 2013, 11, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Prem, K.; Liu, Y.; Russell, T.W.; Kucharski, A.J.; Eggo, R.M.; Davies, N.; Centre, F.T.M.M.; Jit, M.; Klepac, P. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: A modelling study. Lancet Public Health 2020, 5, e261–e270. [Google Scholar] [CrossRef] [Green Version]
- Huang, C.; Liu, X.; Sun, S.; Li, S.C.; Deng, M.; He, G.; Zhang, H.; Wang, C.; Zhou, Y.; Zhao, Y.; et al. Insights into the transmission of respiratory infectious diseases through empirical human contact networks. Sci. Rep. 2016, 6, 31484. [Google Scholar] [CrossRef] [PubMed]
- Lei, H.; Xu, X.; Xiao, S.; Wu, X.; Shu, Y. Household transmission of COVID-19-a systematic review and meta-analysis. J. Infect. 2020, 81, 979–997. [Google Scholar] [CrossRef]
- Zhang, H.; Su, Y.; Xu, S.; Chen, G.; Li, C.; Jiang, R.; Liu, R.; Ge, S.; Zhang, J.; Xia, N.; et al. Asymptomatic and Symptomatic Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infections in Close Contacts of Coronavirus Disease 2019 (COVID-19) Patients: A Seroepidemiological Study. Clin. Infect. Dis. 2021, 73, 553–554. [Google Scholar] [CrossRef]
- Hou, Y.J.; Okuda, K.; Edwards, C.E.; Martinez, D.R.; Asakura, T.; Dinnon, K.H.; Kato, T.; Lee, R.E.; Yount, B.L.; Mascenik, T.M.; et al. SARS-CoV-2 Reverse Genetics Reveals a Variable Infection Gradient in the Respiratory Tract. Cell 2020, 182, 429–446. [Google Scholar] [CrossRef]
- Advice on the Use of Masks in the Context of COVID-19 | United Nations in Ethiopia, United Nations. Available online: https://ethiopia.un.org/en/48687-advice-use-masks-context-covid-19 (accessed on 29 January 2022).
- Zhang, R.; Li, Y.; Zhang, A.L.; Wang, Y.; Molina, M.J. Identifying airborne transmission as the dominant route for the spread of COVID-19. Proc. Natl. Acad. Sci. USA 2020, 117, 14857. [Google Scholar] [CrossRef]
- Russell, F.M.; Greenwood, B. Who should be prioritised for COVID-19 vaccination? Hum. Vaccines Immunother. 2021, 17, 1317–1321. [Google Scholar] [CrossRef]
- Yang, J.; Zheng, W.; Shi, H.; Yan, X.; Dong, K.; You, Q.; Zhong, G.; Gong, H.; Chen, Z.; Jit, M.; et al. Who should be prioritized for COVID-19 vaccination in China? A descriptive study. BMC Med. 2021, 19, 45. [Google Scholar] [CrossRef]
- Priority Groups for Coronavirus (COVID-19) Vaccination: Advice from the JCVI. 30 December 2020. Available online: https://www.gov.uk/government/publications/priority-groups-for-coronavirus-covid-19-vaccination-advice-from-the-jcvi-30-december-2020#history (accessed on 29 January 2022).
- Soiza, R.L.; Scicluna, C.; Thomson, E.C. Efficacy and safety of COVID-19 vaccines in older people. Age Ageing 2021, 50, 279–283. [Google Scholar] [CrossRef]
- Kiang, M.V.; Chin, E.T.; Huynh, B.Q.; Chapman, L.A.C.; Rodríguez-Barraquer, I.; Greenhouse, B.; Rutherford, G.W.; Bibbins-Domingo, K.; Havlir, D.; Basu, S.; et al. Routine asymptomatic testing strategies for airline travel during the COVID-19 pandemic: A simulation study. Lancet Infect. Dis. 2021, 21, 929–938. [Google Scholar] [CrossRef]
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Zhong, N.S. Clinical Characteristics of Coronavirus Disease 2019 in China. J. Integr. Med. 2020, 328, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Advice for the Public. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (accessed on 29 January 2022).
- Yan, Y.; Bayham, J.; Richter, A.; Fenichel, E.P. Risk compensation and face mask mandates during the COVID-19 pandemic. Sci. Rep. 2021, 11, 3174. [Google Scholar] [CrossRef] [PubMed]
- Various Measures to Facilitate the Elderly to Receive the COVID-19 Vaccine. Available online: https://www.news.gov.hk/chi/2021/08/20210801/20210801_122654_948.html (accessed on 29 January 2022).
- Nationwide COVID Fight Proves Effective. Available online: http://english.www.gov.cn/statecouncil/ministries/202108/14/content_WS61171650c6d0df57f98de6d7.html (accessed on 29 January 2022).
- Director-General’s Ppening Remarks at the Special Session of the World Health Assembly—29 November 2021, World Health Organization. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-special-session-of-the-world-health-assembly---29-november-2021 (accessed on 29 January 2022).
- Prata, D.N.; Rodrigues, W.; Bermejo, P.H. Temperature significantly changes COVID-19 transmission in (sub)tropical cities of Brazil. Sci. Total Environ. 2020, 729, 138862. [Google Scholar] [CrossRef] [PubMed]
- Mecenas, P.; Bastos, R.T.R.M.; Vallinoto, A.C.R.; Normando, D. Effects of temperature and humidity on the spread of COVID-19: A systematic review. PLoS ONE 2020, 15, e0238339. [Google Scholar] [CrossRef]
- Aboubakr, H.A.; Sharafeldin, T.A.; Goyal, S.M. Stability of SARS-CoV-2 and other coronaviruses in the environment and on common touch surfaces and the influence of climatic conditions: A review. Transbound. Emerg. Dis. 2021, 68, 296–312. [Google Scholar] [CrossRef]
- Mossong, J.; Hens, N.; Jit, M.; Beutels, P.; Auranen, K.; Mikolajczyk, R.; Massari, M.; Salmaso, S.; Tomba, G.S.; Wallinga, J.; et al. Social contacts and mixing patterns relevant to the spread of infectious diseases. PLoS Med. 2008, 5, e74. [Google Scholar] [CrossRef]
- Ubaru, S.; Horesh, L.; Cohen, G. Dynamic graph and polynomial chaos based models for contact tracing data analysis and optimal testing prescription. J. Biomed. Inform. 2021, 122, 103901. [Google Scholar] [CrossRef]
- Li, J.; Long, X.; Zhu, C.; Wang, R.; Hu, S.; Wang, T.; Li, J.; Lin, Z.; Xiong, N. Management of a Parkinson’s disease patient with severe COVID-19 pneumonia. Ther. Adv. Chronic Dis. 2020, 11, 2040622320949423. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).